Documentation must be received by CGS within calendar days for review and payment determination. Any claim submitted to CGS may be selected for medical review and generate an MR ADR. If you decide to appeal Write your Medicare Number on all documents you submit with your appeal request. Keep a copy of everything you send to Medicare as part of your appeal. What is the Medicare appeal process?
How do you appeal a Medicare drug plan? Make sure you review the ADR letter carefully as the ADR letter may request multiple types of documentation. CMS guidelines require providers to submit documentation within days of the ADR date. If you need to change the address we have for you to receive ADRs, please complete a CMS-8enrollment form. After an ADR is received and documentation submitte if it is determined that the service should be denied and the provider submits an appeal resulting in payment , does this denial become a Comprehensive Error Rate Testing (CERT) error ? Additional documentation request (ADR) 1. Refer to your request letter for the specific time frame.
Always return your documentation to the Medicare contractor identified in the ADR. Since different contractors may use very similar-looking letters, pay close attention. The websites for the respective QIC jurisdictions contain instructions to stakeholders for electronic (e.g., fax or portal) submission of reconsideration requests or documentation. Guidance regarding the options for submitting reconsiderations and related documentation is also summarized by QIC jurisdiction in the table below.
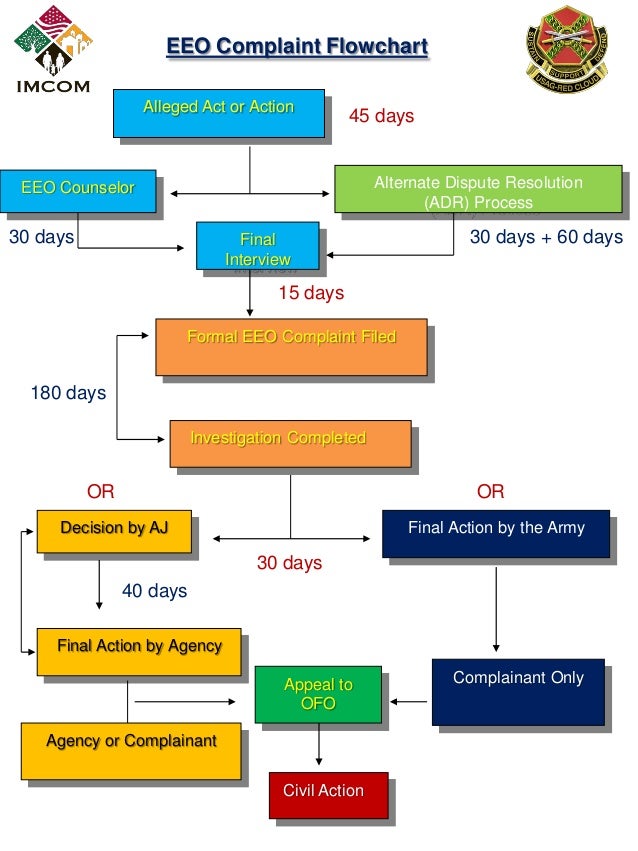
Note: implementation of these alternative mechanisms does not preclude CMS stakeholders from ongoing submission of 2ndlevel appeals via hard copy mail. Another ongoing, alternative method to submit electronic 2nd level Medicare FFS Part A and H. See full list on cms. Once an initial claim determination is made, any party to that initial determination, such as beneficiaries, providers, and suppliers – or their respective appointed representatives – has the right to appeal the Medicare coverage and payment decision. For more information on who is a party, see CFR 405. Second Level of Appeal:Reconsideration by a Qualified Independent Contractor (QIC) 3. Third Level of Appeal:Decision by the Office of Medicare Hearings and Appeals (OMHA) 4. Fourth Level of Appeal:Review by the Medicare Appeals Council 5. A representative may be appointed at any time during the appeals process.
Create a written notice containing all of the elements listed in CFR 405. There are ways that a party can appoint a representative: 1. The appointment of representative is valid for one year from the date it contains the signatures of both the party and the appointed representative. A valid appointment of representative may be used multiple times to initiate new appeals on behalf of the party, unless the party provides a written statement of revocation of the representative’s authority. Home Health Agencies (HHAs), Skilled Nursing Facilities (SNFs), Comprehensive Outpatient Rehabilitation Facilities (CORFs), and Hospices caring for beneficiaries enrolled in Original Medicare are required to notify beneficiaries of their right to an expedited review process when these providers anticipate that Medicare coverage of their services will end before they have finished providing them. Hospitals are also required to notify hospitalized inpatient Original Medicare beneficiaries of their hospital discharge appeal rights and their right to appeal a discharge decision.
Applicable regulations can be found at 42. For detailed information about the expedited determination appeals process, see the CMS. Beneficiaries in traditional Medicare have a legal right to an Expedited Appeal when home health providers plan to discharge them or discontinue Medicare -covered skilled care. Look for documentation outside the medical record. However, the NAC never adds that MDS note as a progress note, and the.
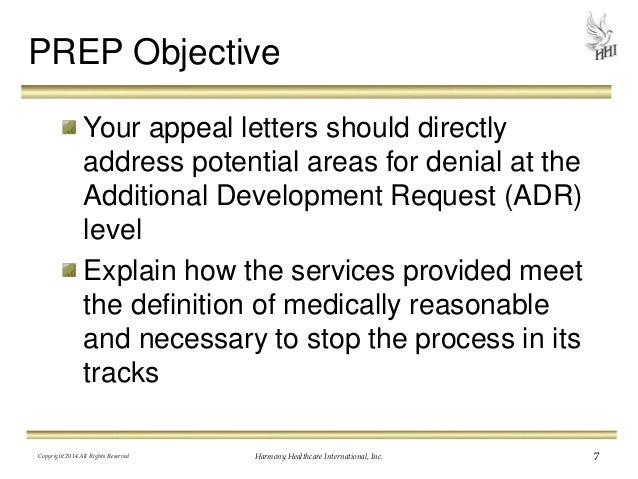
Follow the auditor’s rules and organize logically. Understand what the auditor is asking for, and give it to them. The Current Medicare Part A Appeal Process Request for Reconsideration.
The Medicare Part A “request for reconsideration” procedure entitles an individual who is a. A hospice provider has a right to a hearing regarding any. These can be triggered during the billing process with several line items on the UB-serving as a catalyst or through coded items on the MDS assessment which is transmitted to the State and Federal database. ADR and Appeals Management.
In the past few years, the home health and hospice industry has experienced more scrutiny from regulatory and payer sources than in the history of the industry. Each claim, including all documentation requeste must be faxed individually for proper identification of claims. In a Medicare Advantage plan, your case is automatically referred to the second level of appeal if the level decision goes against you.
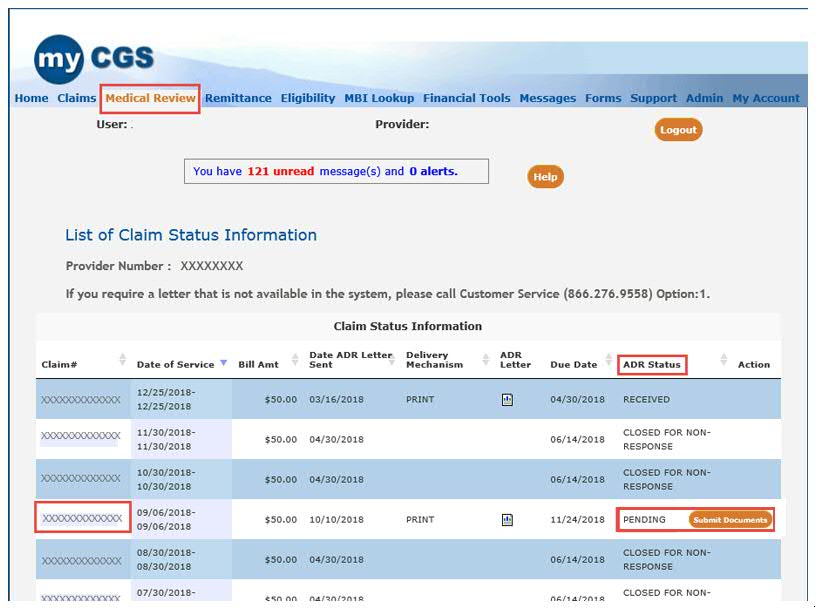
In a Part D plan, you can request a level reconsideration within days of the date of the plan’s decision. Reconsideration by a QIC 3. Redetermination by a MAC 2. Review by the Medicare Appeals Council, within the Department Appeals Board 5. Hearing by an Administrative Law Judge (ALJ) 4. Mailing addresses for certain additional documentation requests (ADRs) have changed. Carefully review your ADR letter to ensure your sending medical documentation to the correct address to avoid delays.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.