I am requesting a hearing to resolve this matter. Instructions for completing the sample appeal letter : 1. Please customize the appeal letter template based on the medical appropriateness. Fields required for customization are in RED. It is important to provide the most complete information to assist with the appeal of a prior authorization denial. The appellant (the individual filing the appeal) has 1days from the date of receipt of the redetermination decision to file a reconsideration request.
The redetermination decision can be communicated through a Medicare Redetermination Notice (MRN), a Medicare Summary Notice (MSN), or a Remittance Advice (RA). The redetermination decision is presumed to be received days after the date on the notice unless there is evidence to the contrary. A reconsideration must be requested in writing. Send a written request containing all of t. See full list on cms.
If a MAC has dismissed a redetermination request, any party to the redetermination has the right to appeal a dismissal of a redetermination request to a QIC if they believe the dismissal is incorrect. The request for review must be filed with the QIC within days after the date of receipt of the dismissal. When the QIC performs its review of the dismissal, it will only decide on whether or not the dismissal was correct.
If it determines that the MAC incorrectly dismissed the redetermination, it will vacate the dismissal and remand the case to the MAC for a redetermination. NOTE: A QIC’s action after review of a MAC’s dismissal of a redetermination request is binding and not subject to any further review or appeal. A QIC may dismiss a reconsideration request in the following instances: 1. If there are certain defects, such as 2. The party fails to file the request within the appropriate timeframe and did not show (or the QIC did not accept) good cause for late filing 2. The representative is not appointed properly 2. The requestor is not a proper party Detailed information on QIC dismissals can be found at CFR 405.
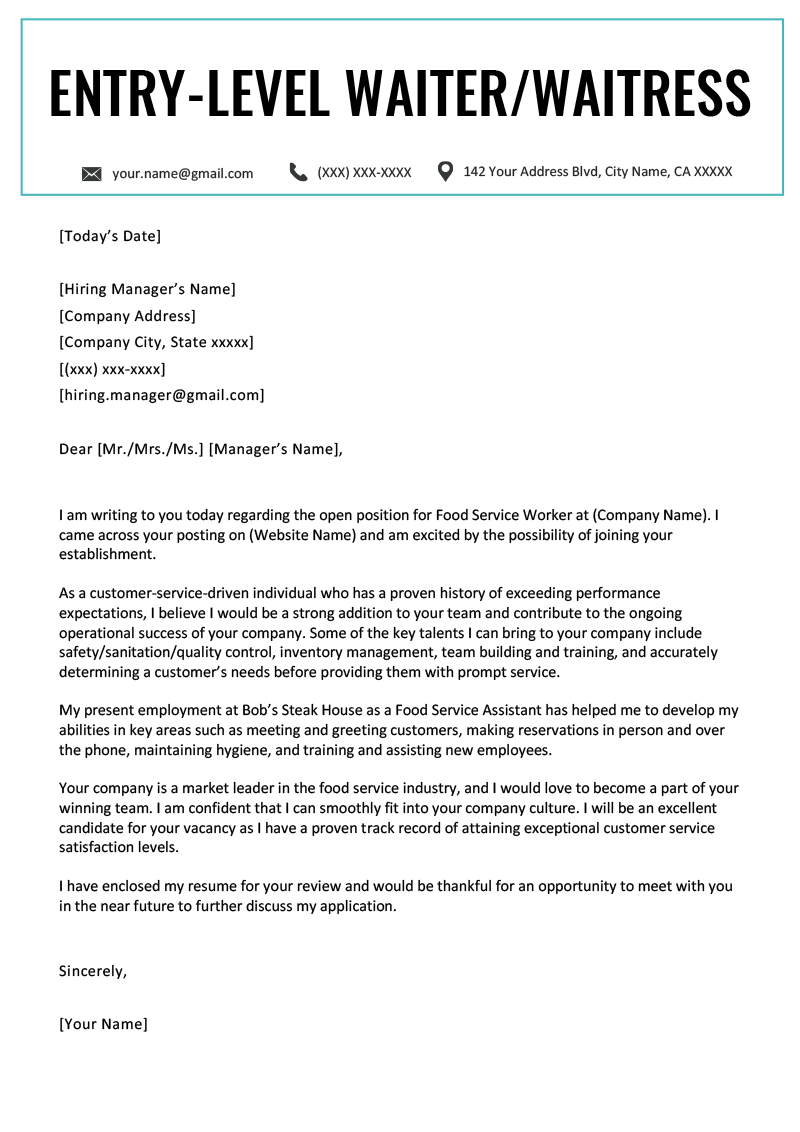
Request review of the dismissal by an Administrative Law Judge (ALJ,) or attorney adjudicator at the Office of Medicare Hearings and Appeals (OMHA) 2. What is a sample appeal letter? Why you should write a strong appeal letter? It is for an employee who has been denied a raise. Use this sample to help you write your appeal letter. Be sure to revise the sample to fit your particular situation.
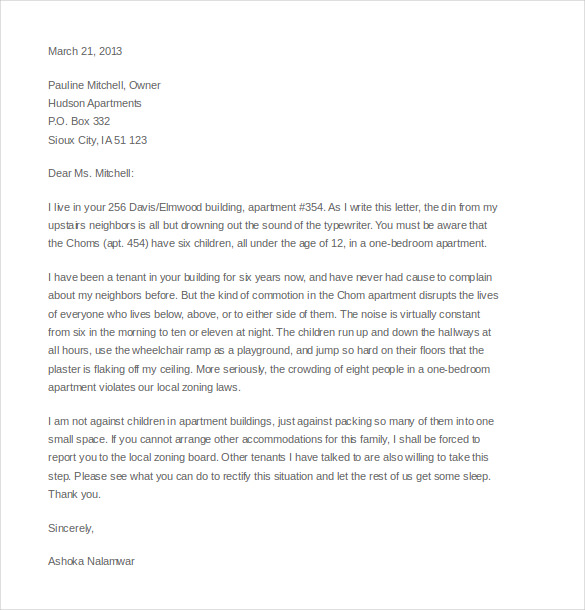
Appeals are most likely to be successful when presented in accordance with the plan’s appeals process and timeframe. The most effective appeal letters are very clear statements about the purpose of the letter , factual and brief. There are a few things that an appeal letter needs to include. Things like the policy number are helpful to allow them to quickly access the account.
They may also need any group numbers or a claim number that has been assigned to the case. While this letter may be included in a doctor’s letter that is attached for documentation, it helps to summarize and put things in a quick and readable format. Was the decision a result of an error on behalf of the insurance company?

If you believe this was a mistake, state the correct information that may make all the difference in whether the claim will be approved or denied. It is not uncommon for a coding error to have taken place. For instance, the insurance company may have you down as receiving one prescription medication when actually it was another one. Make sure to state why you believe they made the wrong decisions.
If you need to go out of network to get the services you nee explain yourself well and attach any documentation necessary. The whole purpose of the letter is to ask for reconsideration. Before drafting an appeal letter, make sure to have property documentation and be ready to answer questions and fill out any packets the insurance company may ask.
The details as to why my home is over assessed are given below. In your appeal letter , be sure to include the claim number, patient name and ID number, the date of service, and the amount billed. Begin the body of the letter by outlining your expectations for claim settlement.
Then explain why the claim should pay per the expectations you describe. If an initial appeal is rejected: There can be multiple levels of appeal. Each of the appeal letters can be adapted for higher level appeals.
After a second - level appeal , additional adjudication may include review by an independent noninsurance-affiliated external review board or hearing. PPMD has worked with parents (thank you Lori Ware!) and providers in our community to develop sample templates for letters of appeal for parents, physical therapists and medical providers. These templates include space for professional review and recommendations, as well as space for personalization. Typically you have 1days from the date of the denial to file your first- level appeal. Appeal filing deadlines are very important.
If your insurance company upholds its denial, you may have to file a second - level appeal before proceeding to external review (if available). The second - level deadlines can be much shorter. It can be for academic, legal, business, or medical purposes.
There may be different in terms of the appeal explanation, but all of them have the same functions. We have available Letter Templates that will guide you on your writings. Provider Claim Dispute Request – Second Level INSTRUCTIONS: This form must be returned within months (months for Medicare) from the date on the applicable Remittance Advice to initiate the claim dispute process. Use one form for each disputed claim.
CalOptima Grievance and Appeals Resolution Services.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.