Florida, Puerto Rico, and U. MEDICARE RE DETERMINATION REQUEST FORM — 1st LEVEL OF APPEAL. Beneficiary’s name (First, Middle, Last) Medicare number. Medicare Advantage plans: appeals for nonparticipating providers. In order to request an appeal of a denied claim, you need to submit your request in writing within calendar days from the date of the denial. How long does a Medicare appeal take?
How do I file an appeal to a Medicare claim? How to appeal a claim denied by Medicare? You have one year from the date of occurrence to file an appeal with the NHP.
We are currently in the process of enhancing this forms library. Therapy Authorization Forms Specific forms for each therapy and instructions for completion. Line of business: ☐ Marketplace ☐ Medicaid ☐ Medicare Today’s Date. Do not use this form for an appeal being submitted on behalf of the member for a denied prior authorization before the service has been performed. Grievances do not include claims or service denials, as those are classified as appeals.
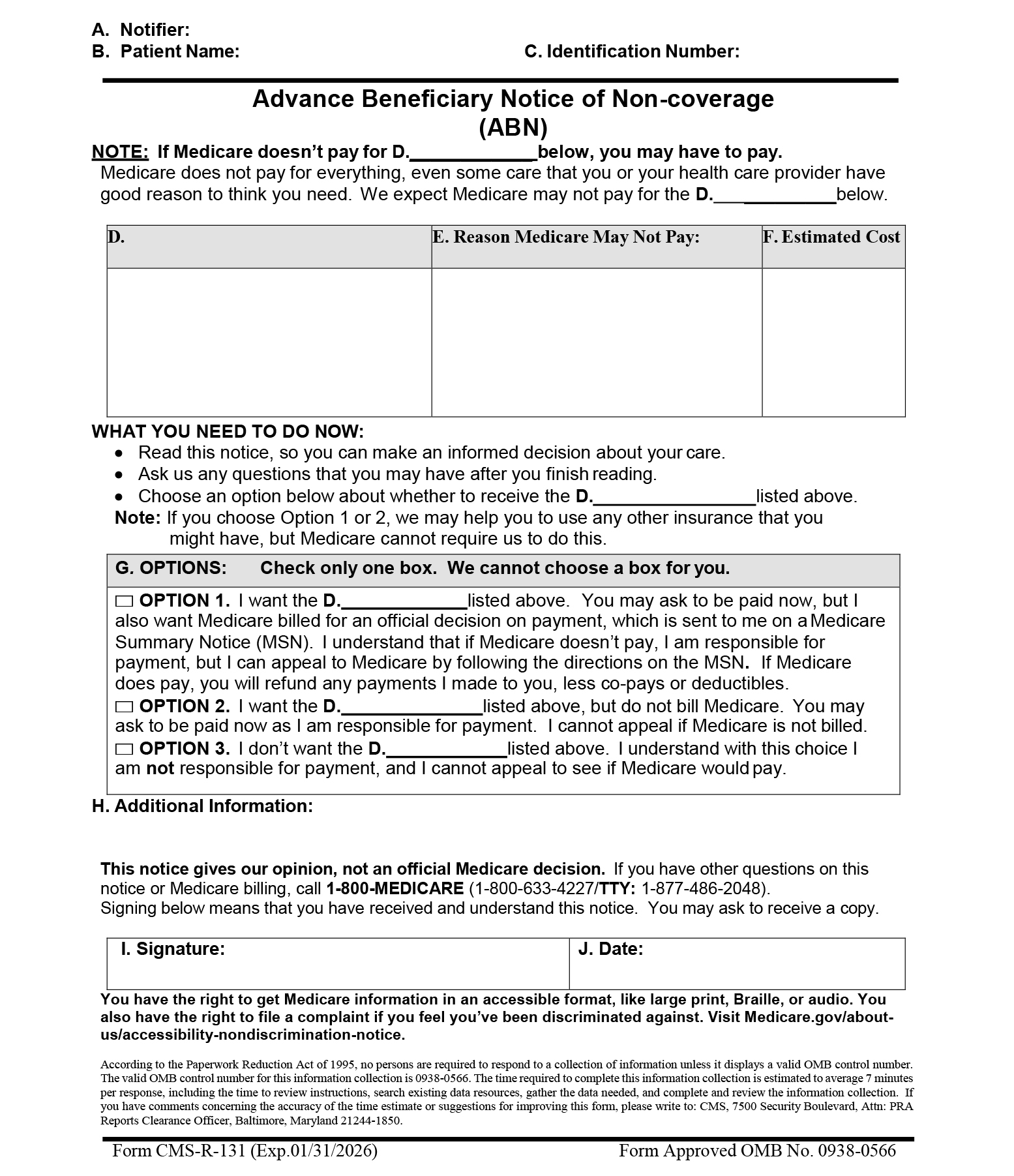
It describes how the Medicare appeals. In this booklet, “I” or “you” refer to Medicare beneficiaries, parties, and appellants participating in an appeal. The following forms are designed for Part B providers who submit claims to CGS. All forms are in the Portable Document Format (pdf). Follow the instructions for sending an appeal.
Fax or mail the form. Download our Standard Medicare appeal letter templates to help you more quickly submit an appeal and ensure you include all necessary information the first time. There is an appeal letter template for each of the five levels of a Standard Medicare appeal process. Access each through the Other Formats section on this page. Prior Authorization Request Forms.
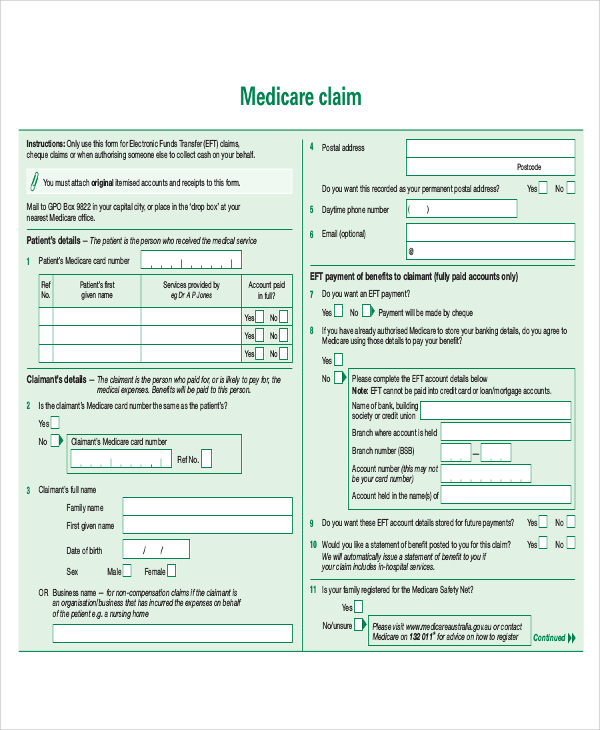
HMO SNP Drug Coverage Determination Form (PDF) Medicare Links (PDF) - (Please note: By clicking on the links below you will be leaving the Superior HealthPlan website.) Ambetter Forms. Appeals Information section of the MSN. Mail or fax the letter or completed form to UnitedHealthcare. This appeal process applies to all of our medical benefits plans. Reconsideration requests must be submitted in the form of a letter.
State requirements take precedence when they differ from our policy. Find out how to appeal a payment. Request for redetermination of Medicare prescription drug denial - Providers and members can use this form to request a redetermination ( appeal ) of a Medicare prescription drug denial. Waiver of liability - Include this form with your appeal if you are a non-participating provider. If you have received an adverse determination AND the member is still hospitalize please call the regional UM department to provide additional information for review.

If you received a Medicare Redetermination Notice (MRN) on this claim DO NOT use this form to request further appeal. There is a limit of one appeal per denial §All provider appeals have a standard turn-around time of days. PCP referral form - Use when referring a member to a specialist. Care management forms. Patient notice of medicare.
Submit your request for a standard appeal in writing by fax, mail, or online through the Kaiser Permanente member website (see below for contact information). If you need a fast appeal due to a life-threatening situation, call us. This form should be completed by providers for payment appeals only. Your card is paper, which is easier for many providers to use and copy.
An if you have a Medicare drug plan, be sure to keep that card as well.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.