
You may also submit additional evidence at a later time, but all evidence must be received prior to the issuance of the redetermination. I do not have evidence to. Your next level of appeal is a Reconsideration by a Qualified Independent Contractor (QIC) - Form. MEDICARE REDETERMINATION REQUEST FORM.
A federal government website managed and paid for by the U. Follow the instructions for sending an appeal. File or Directory not found The resource you are looking for might have been remove had its name change or is temporarily unavailable. The appellant (the individual filing the appeal) has 1days from the date of receipt of the redetermination decision to file a reconsideration request.
The redetermination decision is presumed to be received days after the date on the notice unless there is evidence to the contrary. A reconsideration must be requested in writing. Send a written request containing all of t. See full list on cms.
If a MAC has dismissed a redetermination request, any party to the redetermination has the right to appeal a dismissal of a redetermination request to a QIC if they believe the dismissal is incorrect. The request for review must be filed with the QIC within days after the date of receipt of the dismissal. When the QIC performs its review of the dismissal, it will only decide on whether or not the dismissal was correct. If it determines that the MAC incorrectly dismissed the redetermination, it will vacate the dismissal and remand the case to the MAC for a redetermination. NOTE: A QIC’s action after review of a MAC’s dismissal of a redetermination request is binding and not subject to any further review or appeal.
A QIC may dismiss a reconsideration request in the following instances: 1. If there are certain defects, such as 2. The party fails to file the request within the appropriate timeframe and did not show (or the QIC did not accept) good cause for late filing 2. The representative is not appointed properly 2. The requestor is not a proper party Detailed information on QIC dismissals can be found at CFR 405. Please submit one claim per Redetermination request form. When to request a redetermination - A redetermination should be requested when there is dissatisfaction with the original determination.
Your plan must accept any written request for a redetermination from you, your representative, your doctor, or other prescriber. The name of the drug you want your plan to cover. Tip: complete the form electronically and print.
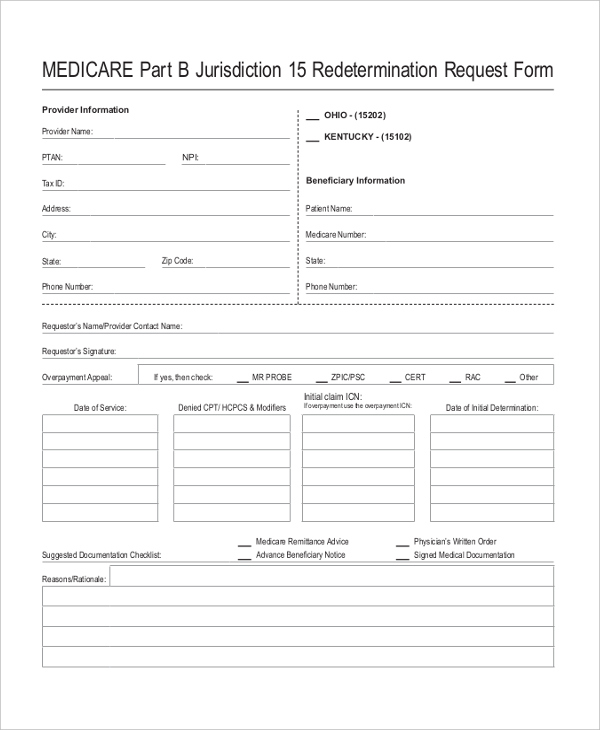
Any redetermination request received that is not completed will be dismissed. However, both the form and all the evidence must be in before your redetermination notice is issued. Medicare Part B JE Redetermination Form. It is equally important that the services submitted as a Reopening are submitted on a reopening request and not a Redetermination request. Their address is listed in the Appeals Information section of the MSN.
Contact Us: Join E-Mail List. The form is for if you disagree with a payment decision made on your medical claim. Corrected claims are not accepted with this form. MEDI-CAL ANNUAL REDETERMINATION FORM You must fill out this form and return it to the county to keep your Medi-Cal!
Busca Más Rápido y Mejor! Submit your appeal request via fax or mail. Appeal, Complaint, or Grievance Form – English, PDF opens new window. Are you requesting a Part A redetermination ? If you decide not to use either of these suggested forms , you must submit, at minimum, the following elements.
Therapy Authorization Forms Specific forms for each therapy and instructions for completion. You may also ask us for a coverage determination by calling the member services number on the back of your ID card. Form must be completed in full, and used only when submitting refund check per claim.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.