Redetermination All Medicaid agencies like TennCare are required to redetermine the eligibility of its members at least once a year. This means TennCare must review members’ information and decide if they still qualify for coverage. About Redetermination. Does TennCare have to redetermine eligibility?
What are the forms of Medicare? If you received a Medicare Redetermination Notice (MRN) on this claim DO NOT use this form to request further appeal. Your next level of appeal is a Reconsideration by a Qualified Independent Contractor (QIC) - Form.
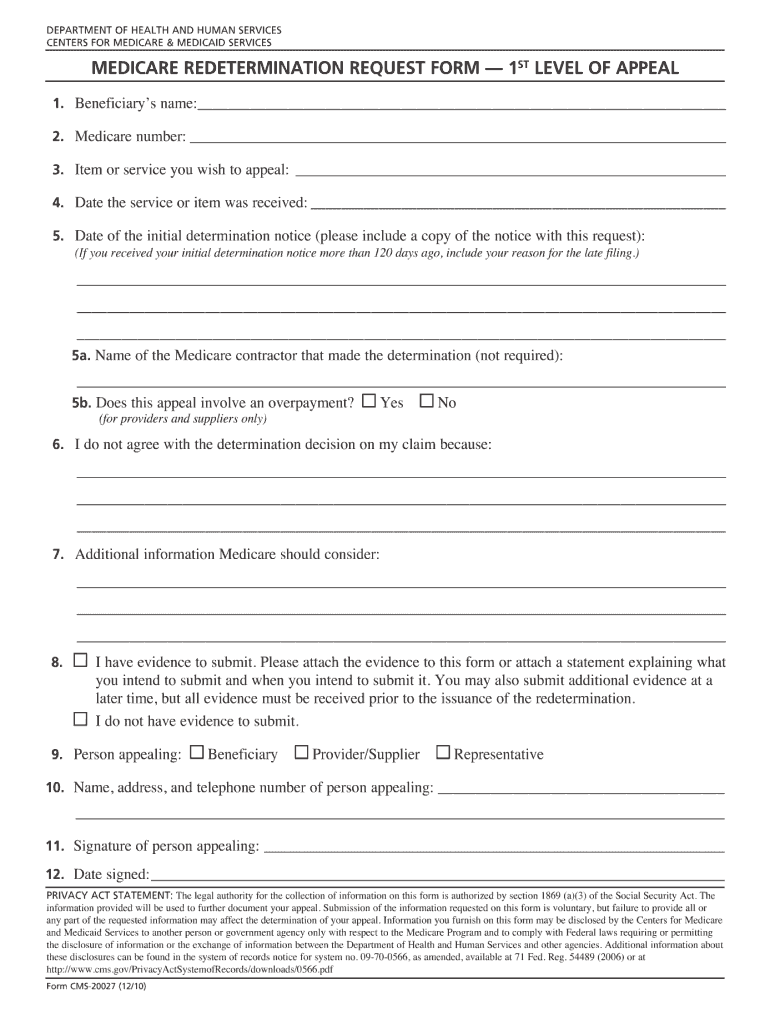
MEDICARE RE DETERMINATION REQUEST FORM — 1st LEVEL OF APPEAL. Beneficiary’s name (First, Middle, Last) Medicare number. Their address is listed in the Appeals Information section of the MSN. Or, send a written request to company that handles claims for Medicare to the address on the MSN.
The clinical editing rationale supporting this database is provided here to assist you in understanding the rationale behind certain code pairs in the database. See full list on palmettogba. CPT is provided “as is” without warranty of any kin either expressed or implie including but not limited to, the implied warranties of merchantability and fitness for a particular purpose. The scope of this license is determined by the AMA, the copyright holder.
Any questions pertaining to the license or use of the CPT must be addressed to the AMA. End Users do not act for or on behalf of CMS. THE CMS DISCLAIMS RESPONSIBILITY FOR ANY LIABILITY ATTRIBUTABLE TO END USER USE OF THE CPT. THE CMS WILL NOT BE LIABLE FOR ANY CLAIMS ATTRIBUTABLE TO ANY ERRORS, OMISSIONS, OR OTHER INACCURACIES IN THE INFORMATION OR MATERIAL CONTAINED ON THIS PAGE. In no event shall CMS be liable for dir.
Compare Affordable Plans in Your Area. Find the Plan That’s Right For You. Since your request for coverage of (or payment for) a prescription drug was denie you have the right to ask us for a redetermination (appeal) of our decision.
You have days from the date of our Notice of Denial of Medicare Prescription Drug Coverage to ask us for a redetermination. Please complete the form below and click submit. You, your physician or your representative need to send a letter or complete a Request for Prescription Redetermination Form and contact us. However, both the form and all the evidence must be in before your redetermination notice is issued. Appeal through your Medicare Summary Notice (MSN) A second way to make a redetermination appeal is through your Medicare Summary Notice (MSN).
An Appointment of Representative form or other legal documentation authorizing you to act on the covered person’s behalf (if you are filing an appeal on behalf of a covered person) Please note that the commercial plan appeals process is the same for nonparticipating and participating providers. Check the box that most closely describes your appeal or reconsideration reason. Complete the top section of this form completely and legibly. Be sure to include any supporting documentation, as indicated below. Requests received without required information cannot be processed.
CGS provides a variety of services for Medicare beneficiaries, healthcare providers, and medical equipment suppliers in states, supporting the needs of over million Medicare beneficiaries and 100healthcare professionals nationwide. This is called a redetermination or an appeal. Use this form to send us your appeal. When we denied your drug, you received a Notice of Denial of Medicare Prescription Drug Coverage.
Who may request an appeal. You may ask us for an appeal. BlueCare Plus Tennessee , an Independent Licensee of the BlueCross BlueShield Association BlueCare Plus Tennessee is an HMO SNP plan with a Medicare contract and a contract with the Tennessee Medicaid program. Enrollment in BlueCare Plus Tennessee depends on contract renewal.
Redetermination (Appeal) This section describes how you can exercise your appeal rights under the Medicare Part D benefits of your Bright Health Medicare Advantage plan. We understand that healthcare is personal and can be complicated – that’s why we’ve put together the following Medicare Part D Redetermination QA for you to use. Because we, denied your request for coverage of (or payment for) a prescription drug, you have the right to ask us for a redetermination (appeal) of our decision. If First Choice VIP Care Plus denies to cover or pay for a prescription drug, you or your representative can ask us to review our decision.
Because we, Blue MedicareRx (PDP), denied your request for coverage of (or payment for) a prescription drug, you have the right to ask us for a redetermination (appeal) of our decision. If you do not wish to appeal a medical decision online, you can use the Form SSA-56 Request for Reconsideration.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.