
How do I file an appeal ? You’ll get your MSN every months if you get any services or medical supplies during that 3-month period. If I need to change my address:Contact Social Security. If you get RRB benefits, contact the RRB. Keep your receipts and bills, and compare them to your MSN to be sure you got all the services, supplies, or equipment listed.
See full list on medicare. You, your representative, or your doctor must ask for an appeal from your plan within days from the date of the coverage determination. The MSN is not a bill. Instead of an MSN, you will receive an Explanation of Benefits (EOB) or a Notice of Denial of Payment.
If your appeal is denie you may file another appeal with an independent contractor,. An appeal is a formal request you make if you disagree with a coverage or payment decision. Details on the applicable notices and forms are available below (including English and Spanish versions of the standardized notices and forms). This notice gives you a summary of your prescription drug claims and costs. Learn more about the EOB.

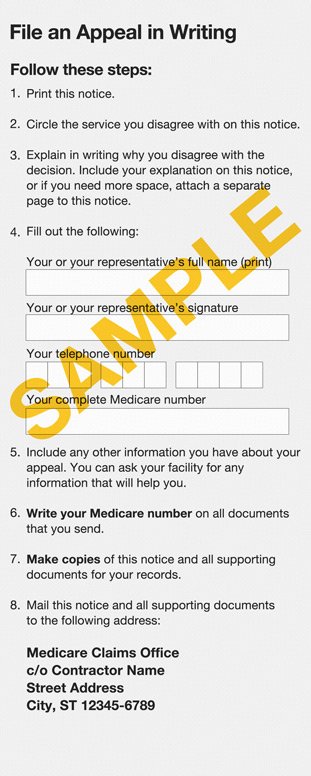
Instant Downloa Mail Paper Copy or Hard Copy Delivery, Start and Order Now! You have only 1days to appeal these denials. These financial liability and appeal rights and protections are communicated to beneficiaries through notices given by providers. MSN explains the status of your recent healthcare claims. You can file an appeal by submitting a Redetermination Request form to the company on the last page of your MSN.
Simply follow these instructions in order to file. There is not a minimum monetary threshold at the first level of appeal , so you can ask for a redetermination no matter how low cost your medical claim. An MSN is not a bill. Though you may keep your MSNs throughout the year, eventually, you will need to dispose of your MSNs.
Medicare Summary Notice disposal. In writing, provide your decision to appeal the denial. You can appeal a denial immediately upon receipt of a notice indicating coverage is denied.
It notifies them of action taken on their processed claims. CMS concurrently gives notice of the termination to the public. Appeal by the provider. Members must file their appeal within calendar days from the date included on the notice of the coverage decision.
Exceptions may be granted if you have a good reason for missing the deadline. To begin a standard appeal , a claim for all of the subsequent services must be submitted. It also contains other helpful information for beneficiaries. You must file an appeal within months of the date of the denial notice.
For more information, please see our privacy notice. For example, it might say that the service or item at issue was not “medically reasonable or necessary. You can also send any additional information you may have about your appeal. After you submit your appeal and all supporting documentation, you will receive a decision within days.

Adjustments to the initial claim or resubmissions for the same item or service will not extend or change the appeal rights on the initial determination. A request filed is considered to be filed the date the MAC receives it. Your MSN is not a bill, but you should carefully review it all the same.
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.